CASES IN GENERAL MEDICINE
A 45 yr old male is a chronic alcoholic
since 20 yrs carpenter by occupation was brought to causality in a state of
altered sensorium since 1 day.
Hi, I am Ankesh Kumar Sahu is a medical
student. This is an online E logbook to discuss our patient’s
de-identified health data shared after taking his/her/guardian’s signed
informed consent. This E-log book also reflects my patient-centered online
learning profile and your valuable inputs on the comment box are welcome. I've
been given this case to solve in an attempt to understand the topic of
"patient clinical data analysis" to develop my competency in reading
and comprehending clinical data including history, clinical findings,
investigations, and come up with a diagnosis and treatment plan.
CHIEF
COMPLAINTS
•Difficulty in walking&decreased appetite since 15 days
•Constipation since 5 days
•Fever and pedal edema since 3 days
•Vomiting since 2 days
HISTORY OF PRESENT ILLNESS
•Patient was apparently asymptomatic 6 months
Back until he had b/l pedal edema.he has diagnosed with hypothyroidism
•Patient had difficulty in walking and decreased appetite since then.
•H/o constipation since 5 days.
•Fever - low grade , intermittent , releived with treatment since 3 days.
•B/l pedal edema - pitting , extending upto knees since 3 days.
•Vomiting - non-bilious, non-projectile, associated with food particles since 2 days.
•Altered sensorium since 1 day.
•Not a k/c/o DM/HTN/Asthma/Epilepsy/CAD/TB
HISTORY OF PAST ILLNESS
•1.5 months back he had a history of fever, dry cough&weight loss from then
•1 month back he had tingling&numbness in b/l lower limbs till ankle later he diagnosed as peripheral neuropathy, the patient had difficulty in walking and decreased appetite since then
TREATMENT HISTORY
•He was on T.Thyronorm 25mcg for hypothyroidism
PERSONAL HISTORY
•HE is chronic alcoholic since 20 yrs
FAMILY HISTORY
•No familiar history
GENERAL EXAMINATION
•Patient was in altered sensorium
•Moderately built and moderately nourished
•No Icterus and pallor
•B/l pedal edema
•No lymphadenopathy
ON EXAMINATION
12/07/21
•Pt was in altered sensorium
•Not oriented to T/P/P
•GCS:-E2V2M4
13/07/21
•E2V1M4
•TEMP 98.4°F
14/07/21
•E2V2M4
•Temp 98.4 ° F
•Anisochoria&sluggish reacting to pupil
15/07/21
•E4V4M4
16/07/21
•E1V1M1
VITALS
12/07/21
•PR:86 BPM
•BP:90/50 mmHg
•Spo2:-98% on RA
13/07/21
•BP 120/90 mmHg
•PR -92/min
•Spo2 91 % on RA
14/07/21
•BP 120/90 mmHg
•PR 85/min
•Spo2 -85% on RA
•Spo2-95% on 4 lit
15/07/21
•BP :-110/90 mmHg
•PR:-120/min
•spo2-90% on RA
-95% on 4 lit
16/07/21
•BP :- 80/60 mmHg
•PR -114/min
•spo2-80% on RA
-96% on 4lit o2
CVS
12/07/21
•S1 S2 + ,no murmurs
•RS:BSE+,NVBS
•P/A: Soft, NT
13/07/21
•S1s2 +
•RS:-B/LAE +
•Rt side wheeze in IMA,IAA
•P/A-soft
14/07/21
•S1S2 +
•RS-B/LAE +
•P/A - soft
15/07/21
•S1s2
•RS-B/LAE +
•P/A-soft
16/07/21
•S1S2
•B/LAE +
•P/A -soft
CNS
12/07/21
•Neck stiffness+
•Tone:- Hypotonia in b/l LL
•Power:-
Left UL 3/5
Left LL 1/5
Right UL &LL 0/5
•Reflexes:-
2+, plantar:-withdrawal
13/07/21
Cns Rt Lf
•Tone- UL N N
LL hypo hypo
•Power-UL moving both UL
LL -
•Reflexes B ++ ++
T + +
S + +
K + +
A + +
P + +
14/07/21
Cns RT LT
•Tone - UL N N
LL hypo hypo
•Power -UL moving both UL
LL --
•Reflexes B ++ ++
T + +
S + +
K + +
A - -
P withdrawl
15/07/21
Rt lt
•Tone -UL hypo hypo
-LL hypo hypo
•Power -UL - -
UL - -
•Reflexes
B + +
T + +
S + +
K + +
A + +
P withdrawl
16/07/21
Rt lt
•Tone- UL hypo hypo
LL hypo hypo
•Power - UL - -
LL - -
•Reflexes
B + +
T + +
S + +
K + +
A - -
P withdrawl
INVESTIGATIONS
12/07/21
CUE
APTT
PROTHROMBIN TIME
TROPONIN-1
BLOOD SUGAR RANDOM
SERUM ELECTROLYTES(Na,k,cl)
CREATININE
LIVER
FUNCTION TEST
REPORT
CHEST
RADIOGRAPHY
MRI
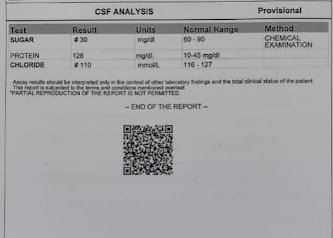
CSF
analysis
INVESTIGATIONS ON 13/07/21
LIVER
FUNCTION TEST
BACTERIAL
CULTURE AND SENSITIVITY REPORT
CYTOLOGY
INVESTIGATIONS ON 14/07/21
PROVISIONAL DIAGNOSIS
•Meningitis-bacterial/TB
•CVA(embolic infarcts in B/L cerebral hemisphere)
•Hyponartemia
•Chronic nutritional hypoalbuminemia
13/7/21
Coronary artery disease
HFIEF(EF 42%)
TREATMENT
12/07/21
1)Inj CEFTRIAXON 2gm × IV ×BD
1-×-1
2)Inj DEXMETHASONE 8mg×IV × BD
1-×-1
3)INJ PAN 40gm × IV × OD
4)IVF NS 100 ml/hr
5)Inj THIAMINE 1 amp in 100 ml NS/IV/OD
6)Inj OPTINEURON 1 amp in 100 ml NS/IV/OD
7)temp charting 4th hrly
8)TAB PCM 650mg ×RT ×sos
13/07/21
1)Inj CEFTRIAXON 2gm × IV ×BD
2)Inj DEXMETHASONE 8mg×IV × BD
3)INJ PAN 40gm × IV × OD
4)IVF NS 100 ml/hr
5)Inj THIAMINE 1 amp in 100 ml NS/IV/OD
6)Inj OPTINEURON 1 amp in 100 ml NS/IV/OD
7)temp charting 4th hrly
8)T.ISONIAZID -300 mg - 1 tab/day
T.RIFAMPSIN -600 mg-2 tab/day
T.PYRIZINAMIDE-1500 mg -2 tab/day
T.ETHAMBUTOL-900 mg -800mg - 1 tab / day
100mg-1/day
9)TAB ASPIRIN 150mg × RT×OD
10)TAB ATORVAS 40 mg ×RT ×OD
14/07/21
1)Inj CEFTRIAXON 2gm × IV ×BD
2)Inj DEXMETHASONE 8mg×IV × BD
3)FLUID RESTRICTION 1.5 lit /day
4)RT feeds
100ml milk & 3 to 4 scoops protein powder -4th hrly
100ml free water -2nd hrly
5)INJ PAN 40gm × IV × OD
6)Inj THIAMINE 1 amp in 100 ml NS/IV/OD
7)Inj OPTINEURON 1 amp in 100 ml NS/IV×OF
8)IVF 3% Nacl @ 10ml/hr
9)T.ISONIAZID -300 mg - 1 tab/day
T.RIFAMPSIN -600 mg-2 tab/day
T.PYRIZINAMIDE-1500 mg -2 tab/day
T.ETHAMBUTOL-900 mg -800mg - 1 tab / day
100mg-1/day
10)TAB ASPIRIN 150mg × RT×OD
11)TAB ATORVAS 40 mg ×RT ×OD
12)TAB TOLVAPTAN 15 mg × RT × OD
13)TAB THYONORM 25 MCG × RT × OD
14)NEBULISATION
ipravent -6th hrly
Budecort 6th hrly
mucomist 6th hrly
15) oral suction 2nd hrly
16) position change 2nd hrly
17)TAB BENADON plus 40mg ×RT ×OD
15/07/21
1)RT feeds
100ml milk & 3 to 4 scoops protein powder -4th hrly
2)IVF 3%Nacl @100ml /hr
3)FLUID restriction <5 lit /day
4)Inj CEFTRIAXON 2gm × IV ×BD
5)Inj DEXMETHASONE 8mg×IV × BD
6)INJ PAN 40gm × IV × OD
7)Inj THIAMINE 1 amp in 100 ml NS/IV/OD
8)Inj OPTINEURON 1 amp in 100 ml NS/IV×OF
9)T.ISONIAZID -300 mg - 1 tab/day
T.RIFAMPSIN -600 mg-2 tab/day
T.PYRIZINAMIDE-1500 mg -2 tab/day
T.ETHAMBUTOL-900 mg -800mg - 1 tab / day
100mg-1/day
10)TAB ASPIRIN 150mg × RT×OD
11)TAB ATORVAS 40 mg ×RT ×OD
12)TAB TOLVAPTAN 15 mg × RT × OD
13)TAB THYONORM 25 MCG × RT × OD
14)NEBULISATION
ipravent -6th hrly
Budecort 6th hrly
mucomist 6th hrly
15) oral suction 2nd hrly
16) position change 2nd hrly
17)TAB BENADON plus 40mg ×RT ×OD
16/07/21
1)RT feeds
100ml milk & 3 to 4 scoops protein powder -4th hrly
2)IVF 3%Nacl @100ml /hr
3)FLUID restriction <5 lit /day
4)Inj CEFTRIAXON 2gm × IV ×BD
5)Inj DEXMETHASONE 8mg×IV × BD
6)INJ PAN 40gm × IV × OD
7)Inj THIAMINE 1 amp in 100 ml NS/IV/OD
8)Inj OPTINEURON 1 amp in 100 ml NS/IV×OF
9)T.ISONIAZID -300 mg - 1 tab/day
T.RIFAMPSIN -600 mg-2 tab/day
T.PYRIZINAMIDE-1500 mg -2 tab/day
T.ETHAMBUTOL-900 mg -800mg - 1 tab / day
100mg-1/day
10)TAB ASPIRIN 150mg × RT×OD
11)TAB ATORVAS 40 mg ×RT ×OD
12)TAB TOLVAPTAN 15 mg × RT × OD
13)TAB THYONORM 25 MCG × RT × OD
14)NEBULISATION
ipravent -6th hrly
Budecort 6th hrly
mucomist 6th hrly
15) oral suction 2nd hrly
16) position change 2nd hrly
17)TAB BENADON plus 40mg ×RT ×OD


































Comments
Post a Comment